Delivery of Nucleic Acids Using Polymers
The medical application of molecular nanotechnology, referred to as “nanomedicine,” is believed to lead to progress in human therapeutics in terms of improving health at the molecular scale.1 This has great potential for accessing the currently “undruggable” targets2 with new and smart medicines equipped with high bioavailability and few side effects. Nanomedicines are expected to have a variety of implications in treatment3 and diagnosis,4 which is expressed in the neologism as “theragnostics.”5 While nanotechnology enables diagnosis at the single-cell and molecular level, nanomedical therapeutics are expected to be specifically or even personally tailored. The field of nanomedicine has been developed strongly in the last decade. In particular, advanced drug delivery systems (DDS) have seen attention from multiple disciplines6 to control the pharmacokinetics, toxicity, immunogenicity, biorecognition, and efficacy of the drug.7 Drug carriers can be soluble or insoluble polymers that are formulated as nanoparticles using techniques such as the solvent displacement8 or solvent evaporation/emulsion technique,9 biopolymers,10 or dendrimers.11 Other formulations include polymer complexes,12 “dendriplexes”,13 liposomes,14 micelles,15 and nanogels.16 This review will focus on the sub-sector of drug delivery concerning the delivery of nucleic acids, with a particular focus on poly(ethyleneimine).
Non-viral Delivery of Nucleic Acids
In contrast to highly efficient viral delivery vectors, non-viral counterparts bear less immunostimulatory, mutagenetic, and oncogenic complications; some can approach transfection efficiencies comparable to viruses.17 Therapeutic nucleic acids of interest for nanomedicine can be DNA in plasmids (pDNA), antisense oligonucleotides (AONs), ribozymes, DNAzymes, and more recently, siRNA and shRNA. While pDNA is used in gene therapy to deliver missing genes or replace dysfunctioning genes, all of the other therapeutic nucleic acids down-regulate gene expression by post-transcriptional gene silencing. This also explains their different target compartments: pDNA and shRNA expression vectors need to be delivered into the nucleus for transcription, whereas the cytosol is the site of action of AONs, ribozymes, DNAzymes, siRNA, and shRNA. Unfortunately, cells lack an efficient uptake mechanism for nucleic acids. Spontaneous intracellular translocation that retains bioactivity of the macromolecules is unlikely since nucleic acids are labile, negatively charged biomacromolecules. This has generated interest in research focused on protective formulation of nucleic acids into smart nanodevices that have high transfection efficiencies.
Delivery vehicles for nucleic acids that will make it from bench to bedside need to possess biocompatibility and robust processes of assembly, conjugation, and purification.6 A broad variety of lipid-based vectors, polymers, biopolymers, dendrimers, polypeptides, and inorganic nanoparticles have been investigated by groups all around the world.18 The most prominent polymeric vector is certainly poly(ethyleneimine) (PEI) (Product No. 764582), which is commercially available or can be polymerized as low- or high-molecular weight PEI.19 PEI was first introduced as non-viral gene delivery vector by Bousif, et al. in 1995,20 who described its outstanding property the “proton-sponge-effect.” While liposomes escape the endo/lysosomal compartment after endocytosis due to fusogenic properties, PEI is believed to attract an influx of chloride and, subsequently, an osmotic influx of water into the lysosome as it is protonated. This leads to swelling and bursting of the lysosomes which release the polymer and nucleic acid into the cytosol.
Unfortunately, almost all polymeric vectors have one thing in common: they either form positively charged or amphiphilic complexes with nucleic acids that cause toxicity by interaction with negatively charged cell membranes,21 or cellular components and pathways after successful intracellular entry.22 There seems to be a correlation between transfection efficiency and toxicity up to the point where cells no longer survive. Since it has been reported that low molecular weight (LMW) PEI (Product No. 764604) is significantly less toxic than high molecular weight counterparts,23 a recent study investigated reversible disulfidebased crosslinking of LMW PEI24 to achieve macromolecular vectors. A common principle for decreasing the surface charge of polycation–nucleic acids composites and their non-specific charge-dependent interactions was adopted from “stealthR liposomes” that are surface-modified with poly(ethylene glycol) (PEG) or other hydrophilic compounds, such as carbohydrates.14 This steric stabilization decreased self-aggregation and interactions with proteins in biological fluids, and it increased salt and serum stability. Also, recognition and phagocytotic capture by cells of the reticulo-endothelial system (RES) or aggregation within pulmonary capillary beds in vivo was prevented, thereby enhancing their circulation half-lives. Derivatives of PEI with PEG, saccharides, and a monoclonal antibody (mAb) have been reported to yield stable complexes that partly retained their transfection efficiency. In a systematic study, different densities of grafted PEG chains as well as varied PEG chain lengths were investigated, suggesting that surface charge and toxicity decreased as a function of PEGylation. Unfortunately, transfection efficiency also decreased at comparable polymer-to-DNA ratios. Fortunately the low toxicity affords an opportunity to increase the polymer concentration to increase transfection. An even smarter system was recently described where PEG chains are connected via a peptide sequence which is cleaved in the presence of matrix metalloproteinases (MPPs). Thus, the emerging multifunctional envelope-type nanodevices (MENDs) are PEGylated extracellularly and lose the PEG block upon contact with an MPP that cleaves the peptide spacer. As non-specific endocytosis is triggered by interaction of cationic particles with heparin sulfate proteoglycans on the cell surface, a certain amount of positive surface charge of non-viral vectors is favorable. There are extensive publications which report a diversity of PEI modifications, including full deacylation and succinylation of commercially available PEIs, crosslinking of branched HMW PEI, conjugation of melittin, grafting of chitosan, and immobilization on poly-l-lactide (PLLA) films for layer-by-layer assembly of polyelectrolytes. There are also more synthetic approaches to modify PEI, including the synthesis of PEI-alginate composites, amphiphilic and cyclodextrinthreaded triblock copolymers, PEI-cholesterol composites, and alkyl-oligoamine LMW-PEI derivatives. These modifications target enhanced endosomal release, transfection efficiency, pharmacokinetic parameters, and biocompatibility. One particularly interesting modification is the functionalization of PEI with cell-specific ligands to enable conjugation of targeting ligands, which is described below.
Targeted Gene Delivery Using Cell-specific Ligands
Targeted delivery systems are expected to selectively interact with internalizing receptors on certain cell types in a “lock and key” model that eventually triggers receptor-mediated uptake of the delivery system. Therefore, in this approach, non-specific, chargerelated interactions that can also lead to non-specific toxicity are not necessary for efficient delivery. The dilemma that non-toxic, non-viral vectors which display a neutral surface charge are often less efficient than their non-shielded counterparts can be overcome by attaching targeting ligands. As another advantage, selective delivery systems require much lower amounts of siRNA or DNA for the same effect as a result of specific transfection. Targeting approaches exploit the fact that certain receptors are overexpressed on a variety of tissues and especially malignant abnormal cells due to their active proliferation and their demand for nourishment. Therefore, many targeted delivery systems are specific for growth factor receptors and are, therefore, suitable for tumor therapy. A variety of ligands have been used for modification of polymers to increase specificity, reduce the dose, and increase transfection efficiency. Conjugates of PEI are listed in Table 1.
Even though successful targeting of liposomes was described in the literature almost 29 years ago,35 until today cell- or tissuespecific delivery has not been clinically exploited.
There are various further possible ligands and a myriad of further multifunctional PEI-based vectors for known and to-be-determined targets. We previously described specificity and activity of a differently synthesized PEG–PEI-based gene delivery system coupled with a novel peptidomimetic small molecule targeting the integrin receptor alpha ν beta 3.36
Concepts of siRNA Mediated Posttranscriptional Gene Silencing
In 2006, Andrew Fire and Greg Mello were awarded the Nobel Prize in Physiology for their discovery of gene silencing by introduction of double-stranded RNA (dsRNA).37 Their work led to the identification of a catalytic mechanism of a multi-protein complex which incorporates short RNAs that, on their part, are complementary in sequence to mRNA which is subsequently degraded.37 This mechanism is an evolutionary conserved defense process for inactivation of foreign, e.g., transposable, viral, or bacterial genetic information, and it can also be exploited biotechnologically (Figure 1). Long dsRNA, which naturally or directedly reach the cytoplasm, are degraded by “dicer” (an RNase III-like enzyme) into small interfering RNAs (siRNAs) of 21–25 nucleotides in length.38 While long dsRNA can interact with toll-like receptor 3 (TLR3), synthetic short interfering RNA (siRNA) no longer than 19–21 base pairs with 2 nt 3’ overhangs is efficient and lacks interferon response. After being transferred into the cytosol where it is incorporated into the RNA-induced silencing complex (RISC), double-stranded siRNA is cleaved upon activation of RISC, and complementary mRNA can bind to the antisense strand. Argonaute (Ago2), an endonuclease in the RISC, subsequently cleaves the mRNA and leads to down-regulation of target gene expression.
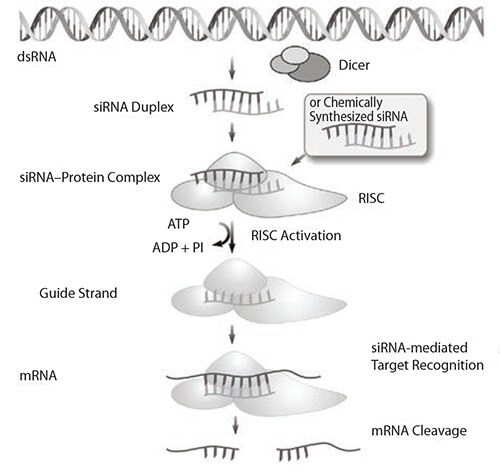
Figure 1.The mechanism of endogenous and induced RNA interference (RNAi). siRNA is eventually incorporated into the RISC where complementary mRNA binds before it is cleaved.
Since the discovery of an RNA interference (RNAi) mechanism in mammalian cells, RNAi is routinely used in functional genomics and drug development. RNA-based therapeutics, on the other hand, are rather sparse. Due to their susceptibility to degradation by ubiquitous nucleases and their strongly negative surface charge, siRNA molecules require effective formulation and cannot easily be compared with small molecule drugs.39 Besides interaction with plasma proteins and degradation by serum nucleases and fast renal clearance in vivo,39 the bottlenecks in efficient RNAi include both translocation of siRNA across the plasma membrane and its subsequent escape from the endosomal/lysosomal compartment. Despite these drawbacks, successful reports on the silencing efficacy of naked siRNA can be found in the literature where siRNA is instilled into the lung or the vagina, or delivered to the liver by high-pressure tail vein injection.40 Most clinical trials involving siRNA-based drugs rely on local administration to the eyes, targeting age-related macular degeneration (AMD) and diabetic retinopathy (Acuity Pharmaceuticals, Alnylam Pharmaceuticals, Inc., and Sirna Therapeutics, Inc.) or direct delivery to the brain or the lung (Alnylam Pharmaceuticals, Inc.). While SIRNA used chemically optimized siRNA in their clinical trial for the treatment of AMD, Alnylam applied cholesterol-attached siRNA targeting the nucleocapsid N gene of the respiratory syncytial virus (RSV), which was successful in their Phase II GEMINI study. Chemical modification of siRNA is not only a means to improve in vivo stability, which has been reported to be a result of modifications of the backbone and/or ribose. The additional benefit of methylation of the ribose 2’ hydroxyl group (2’-OMe) is the diminishing of immunostimulatory effects which have been described after liposomal delivery of siRNA. The knockdown kinetics of unmodified and nuclease-stabilized siRNA were shown to be essentially the same. A promising systemic in vivo application of siRNA is gene silencing in the liver, which can successfully be achieved with so-called “SNALP” (stable nucleic acid lipid particles) formulations.42 Naked siRNA that is systemically applied is known to be excreted via the kidneys faster than it is degraded. Other formulations that have been investigated concerning their in vivo pharmacokinetics are post-PEGylated protamine-lipoplexes, adamantane-PEG-transferrin- bearing cyclodextrin-containing polyplexes, RNA−gold nanoparticle conjugates, chitosan, liposome and PEI-formulated locked nucleic acids (LNAs), and PEG–PEI polyplexes (Figure 2). While post-PEGylation approaches and cholesterol conjugation both extended the circulatory half-life, polyplexes made of pre-PEGylated PEI often have been presumed to disassemble in tissue or circulation.
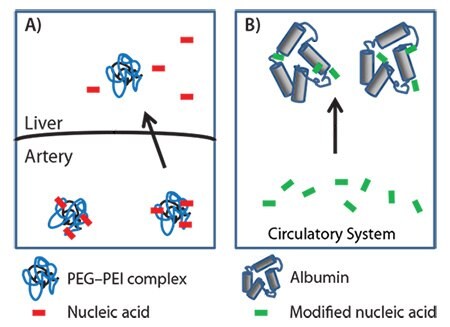
Figure 2.Two delivery methods of nucleic acids are A) intravenously applied complexes of nucleic acids and PEG-PEI, which are suspected to disassemble either in the circulation or upon liver passage, and B) amphiphilic modifications of nucleic acids which bind to albumin.41
Even though RNAi-based knockdown of target mRNA or protein was frequently reported in the literature, none of the pharmaceutical companies had robust delivery systems that would lead to broad clinical translation into RNAi-based therapeutics.
A highly interesting case is CALAA-01, the first experimental therapeutic that provided targeted delivery of siRNA in humans. This case just completed phase I tolerability evaluation of intravenous application in adults with solid tumors refractory to standard-of-care therapies by Calando Pharmaceuticals. CALAA‑01 referred to siRNA against the M2 subunit of ribonucleotide reductase (RRM2) formulated within the RONDEL™ delivery system, a transferrin-targeted cyclodextrin-containing polymer RNAi-nanotherapeutic.
While DNA polyplexes have been extensively studied, there is not as much research published regarding circulatory half-life and biodistribution of siRNA. We previously described the optimization of a method for non-invasive determination of pharmacokinetics and biodistribution of siRNA polyplexes.43 Making use of this optimized method, we then correlated in vivo pharmacokinetics of various (PEG-)PEI/siRNA polyplexes with their in vivo stability, another parameter that is crucially important in the development of polymeric siRNA delivery systems.44
Conclusions and Future Outlook
The field of nanomedicine research developed into several sectors focused on many areas. Poly(ethyleneimine) (PEI) has been a prominent polymer used in the development of three areas in particular: non-viral transfection, targeted delivery, and posttranscriptional gene silencing. In non-viral transfection, research is focused on increasing the efficiency while avoiding toxicity. In targeted delivery, there is a need to develop polymers with a high degree of specificity capable of maintaining a high level of drug activity. The further development of siRNA-mediated gene silencing is dependent on forming stable RNA polyplexes. PEIbased polymers will continue to be an integral part of the further development of these fields.
References
Zaloguj się lub utwórz konto, aby kontynuować.
Nie masz konta użytkownika?