Multiplex your
COVID-19 Work
MILLIPLEX® Multiplex Assays for COVID-19 Research
- MILLIPLEX® Assays for Detection of Human Immunoglobulins Against SARS-CoV-2 Antigens
- MILLIPLEX® Assays for Cytokine Storm-Related COVID-19 Research
- MILLIPLEX® Assays for Emerging COVID-19 Research Areas
- COVID-19 On-Demand Webinars Featuring MILLIPLEX® Kits
- Select Published COVID-19 Studies Using MILLIPLEX® Kits
- References
MILLIPLEX® assays for detection of human immunoglobulins against SARS-CoV-2 antigens
The SARS-CoV-2 coronavirus is the pathogenic cause of the human disease COVID-19. The virus particle consists of RNA encapsulated by the nucleocapsid (N) protein which is enveloped by a membrane (M) protein. The corona-like spike proteins surrounding this inner core consist of subunits S1 and S2, and the receptor binding domain (RBD) which binds to the human cellular angiotensin converting enzyme 2 (ACE2) receptor. Upon binding, the virus enters the cell, takes over the cellular machinery, reproduces, and the viral contagion continues. Viral structural proteins offer the antigenic potential for an immune response. Upon viral infection, the humoral immune system responds first by producing the immunoglobulin IgM, followed later by IgG, which can convey long-lasting immunity. IgA, a mucosal immune response, is also found in blood.
By testing human serum and plasma for IgM, IgG, and IgA antibodies which bind to SARS-CoV-2 antigens, investigators may identify research samples exposed to the SARS-CoV-2 virus exhibiting some level of immune response. Researchers may further understand the immune response throughout infection and recovery from COVID-19.
Each of our three configurable 4-plex panels (Cat. Nos. HC19SERM1-85K, HC19SERG1-85K, and HC19SERA1-85K) allows the researcher to select any or all the following viral antigens: SARS-CoV-2 Spike S1, Spike S2, RBD, and N protein.
Read our Application Note highlighting our MILLIPLEX® multiplex research assays to detect antibodies that recognize SARS-CoV-2 antigenic proteins in human serum and plasma.
For Research Use Only. Not For Use In Diagnostic Procedures.
Example Data
EDTA plasma samples were assayed in duplicate for all four analytes, S1, S2, RBD, and N, according to the protocol in each of the MILLIPLEX® SARS-CoV-2 kits, IgG, IgA, and IgM. Samples were from patient groups testing positive or negative by PCR for SARS-CoV-2 infection: COVID-19 positive “Ventilated” (n=68), COVID-19 positive “Not Ventilated” (n=115), and COVID-19 negative “COVID-” (n=41)1. Graphed assay results show individual MFI for each sample in each group with group means, +/- standard deviation (SD), and p-value significance tests between groups: ****p<0.0001, ***p<0.001, **p<0.01, *p<0.05.
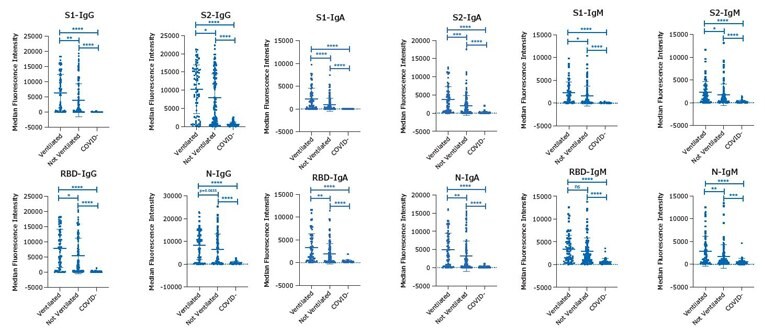
Figure 1.Data for all four analytes, S1, S2, RBD, and N with the MILLIPLEX® SARS-CoV-2 kits, IgG, IgA, and IgM using EDTA plasma samples.
MILLIPLEX® assays for cytokine storm-related COVID-19 research
When the immune system overreacts to a pathogen or other immunogenic substances such as a drug, a hyperinflammatory response may trigger excess production of signaling molecules from immune cells. This is referred to as cytokine storm syndrome (CSS) or cytokine release syndrome (CRS). Acute or systemic inflammation results in fluid buildup in the lungs, respiratory distress, multiple organ failure, and can be fatal.
Human Studies
Recent publications on the cytokine profile in COVID-19 have found elevated levels of M-CSF, IP-10, IL-1RA, IL-10, IL-15, IL-27, TNFα, and IL-8 were predictive of cytokine storm or correlated with more severe disease2,3. In a profiling study, it was found that circulating levels of IL-6, IL-8, TNFα, and IL-10 were associated with severe COVID-19, in addition to IL-18, IP-10, MIG, among others4.
Non-Human Primate Studies
Research on SARS-CoV-2 is also being conducted in non-human primates such as rhesus macaques, which will allow researchers to test possible vaccines and antiviral medications/treatments in relevant animal models. A recent Nature publication used MILLIPLEX® Non-Human Primate assays to analyze serum over multiple time points in macaques with SARS-CoV-2 exposure for changes in cytokine and chemokine levels, and showed increases in IL-1RA, IL-6, IL-10, IL-15, MCP-1, MIP-1β, along with a decrease in TGFα5. Our new MILLIPLEX® Non-Human Primate Cytokine/Chemokine/Growth Factor Panel A allows for simultaneous quantification of 48 immune factors in serum, plasma, and cell/tissue culture supernatant samples. Choose any combination of analytes, customize your premix, or select a 38-plex or 48-plex premixed kit.
Using MILLIPLEX® Multiplex Immunoassays to Understand the Immune Response to COVID-19
Our MILLIPLEX® multiplex immunoassays offer researchers the ability to simultaneously quantitate numerous analytes critical to understanding the immune response in humans. Our 48-plex Human Cytokine/Chemokine/Growth Factor Panel A saves time and sample volume for a snapshot of analyte profiles during a cytokine storm, sepsis, or other disease states. We offer a wide array of MILLIPLEX® soluble protein panels and cell signaling kits to help elucidate the downstream signaling pathways when researching antiviral immune response. Our portfolio offers the widest range of analytes across the most species, including non-human primate panels for vaccine research.
For Research Use Only. Not For Use In Diagnostic Procedures.
Comparison of Sepsis vs. Normal Serum/Plasma Samples Using MILLIPLEX® Human Cytokine Panel A
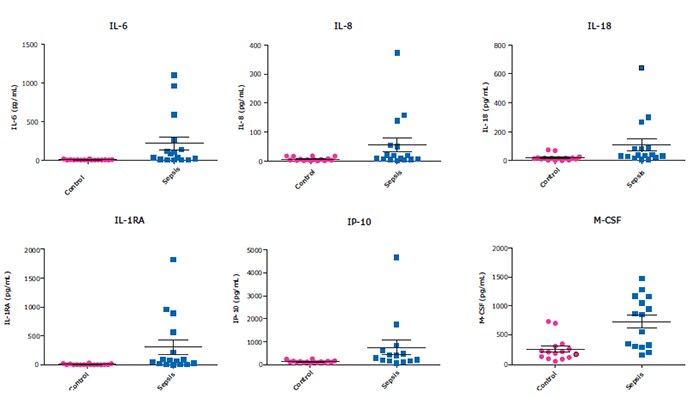
Figure 2.Healthy control (n=20) and sepsis patients (n=16) serum/plasma samples (obtained from BioIVT, Discovery, and BioChemed) were tested neat (25 µL/well) in the HCYTA-60K panel. Shown here is a subset of the analytes which have been mentioned in recent publications to be increased in SARS-CoV-2 cytokine release syndrome (CRS).
For Research Use Only. Not For Use In Diagnostic Procedures.
MILLIPLEX® assays for emerging COVID-19 research areas
ACE and ACE2 play a role in the plasma kallikrein-kinin system (KKS), which controls the blood coagulation system, endothelial cell growth, angiogenesis, the complement pathway, and the renin angiotensin system (RAS)6. Bradykinin, a kinin peptide, along with kallikreins and kininogens make up the KKS. ACE2 functions to decrease bradykinin, and when disrupted, higher bradykinin levels can increase systemic inflammation7. In addition to CSS, the disruption of the RAS/KKS may lead to severe complications in COVID-19. Moreover, the activation of bradykinin receptors mediates inflammation, leading to distinctly elevated cytokine levels. Our MILLIPLEX® multiplex immunoassays offer researchers the ability to simultaneously quantitate numerous analytes critical to understanding these mechanisms triggered by COVID-19, including complement components in our Human Complement Panel 1 (Cat. No. HCMP1MAG-19K ) and Panel 2 (Cat. No. HCMP2MAG-19K ), Renin, Kallikrein-6, and our Human Angiogenesis/Growth Factor Panel 1 (Cat. No. HAGP1MAG-12K ) and Human Angiogenesis Panel 2 (Cat. No. HANG2MAG-12K ).
Coagulopathy is a severe condition that has been associated with COVID-19, indicated by elevated D-dimer levels and extensive microthrombosis in lung autopsies8. Thrombotic complications are associated with multiorgan failure and a higher rate of mortality. Higher levels of acute phase proteins, such as CRP and fibrinogen, have been shown to correlate with this COVID-19 severity. Increased cytokine levels, a hallmark of disease noted previously, can lead to upregulation of adhesion molecules such as ICAM-1, VCAM-1, P-selectin, and e-Selectin9. With our MILLIPLEX® Human Cardiovascular Disease Panel 2 (Cat. No. HCVD2MAG-67K ), ICAM-1, VCAM-1, D-Dimer, and P-selectin can be quantitated simultaneously to study this critical condition.
Your research breakthroughs depend on reliable, high-performing products and services. Our MILLIPLEX® portfolio of immunoassays is the largest portfolio of multiplex biomarker assays, based on Luminex® xMAP® technology, offering you consistent, high-quality results, so you can do your best work while saving time, labor, and cost.
For Research Use Only. Not For Use In Diagnostic Procedures.
COVID-19 On-Demand Webinars Featuring MILLIPLEX® Kits
View our on-demand webinars demonstrating how MILLIPLEX® multiplex assays have been used in COVID-19 research. In these webinars, you will discover how the immune response in COVID-19 patients is assessed and how to successfully integrate multiplex immunoassays into your disease research workflow.
- IgG Antibodies Against SARS-CoV-2 Correlate to Days from Symptom Onset in COVID-19 Positive Patients; Presented by Mary Young, University of Virginia, School of Medicine
- The Dynamics of SARS-CoV-2 Specific Antibody Responses in COVID-19 Patients; Presented by Prof. Dr. Christina S. Falk, Institute for Transplantation Immunology, Hannover
- Immune Responses in Severe COVID-19 Patients; Presented by Prof. Dexi Chen, Beijing Institute of Hepatology
- MILLIPLEX® Multiplex Immunoassays for Use in COVID-19 and Cytokine Storm Research; Presented by Brooke Gilliam, MILLIPLEX® Product Manager
- IL-13 is a Pathogenic Driver of COVID-19; Presented by Alexandra Donlan, University of Virginia
- Keeping COVID-19 at Bay: Existing and Induced Antibody Immunity to SARS-CoV-2; Presented by Dr. Todd Bradley, Children’s Mercy Research Institute
Select Published COVID-19 Studies Using MILLIPLEX® Kits |
|---|
Did you use our MILLIPLEX® products in your paper?
How to Cite Our Products in Your Paper
Ready to publish? We’re happy you’ve used our products to help you move forward in your research!
How to cite MILLIPLEX® assay kits:
- If you are based in the United States or Canada, state MilliporeSigma as the source of your assay.
- If you are based anywhere in the world outside of the United States or Canada, state Merck KGaA, Darmstadt, Germany, as the source of your assay.
- Include the full MILLIPLEX® kit name and kit catalog number, and also list the analytes you used from the kit.
- Include the species of samples you used and how you diluted your samples.
References
To continue reading please sign in or create an account.
Don't Have An Account?